
Dr Mendall is a senior experienced gastroenterologist in practice for nearly 20 years. He is qualified from Cambridge University in 1982 and the Middlesex Hospital in 1985 which distinction.
He is Head of Service for Gastroenterology and Endoscopy at Croydon University Hospital which serves a large and needy population. He is a recognised trainer in gastroenterology and endoscopy and an active researcher with more than 94 peer reviewed publications.
> What happens when you need to see Dr Mendall? > When to consult Dr Mendall?Dyspepsia Explained by Dr Michael Mendall, Consultant Gastroenterologist

Lurking beneath a gut problem may be a plethora of serious conditions....
> Read More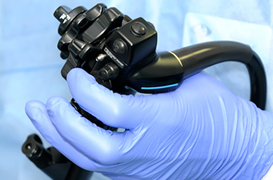
Upper gastrointestinal endoscopy or otherwise known as gastroscopy is used to diagnose a range of oesophageal, stomach and duodenal disorders...
> Read More
A video capsule endoscopy is used to investigate anaemia, where the cause hasn’t been shown by other tests, abdominal pain, and in the assessment of coeliac disease and Crohn’s disease...
> Read More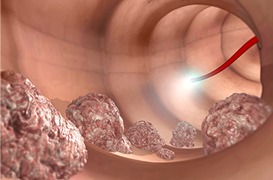
A colonoscopy or telescopic examination of the colon is used to investigate a range of symptoms including abdominal pain, diarrhoea, anaemia, constipation and rectal bleeding...
> Read More